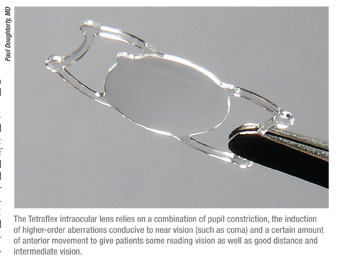
Lenstec’s Tetraflex
The Tetraflex is a hydrophilic acrylic plate lens composed of flexible hydroxyethylmethacrylate (26 percent water) with a UV blocker. It’s got a 5.75-mm optic and 5-degree anterior angulated close-loop haptics. The lens is injected in both eyes through incisions that measure about 2.8 mm. The lens’s approval application is currently under review by the Food and Drug Administration.
The initial idea behind the Tetraflex was to use the IOL’s slight anterior vault to help the lens move forward with accommodative effort, giving improved near vision. However, though the lens moves somewhat, the amount of movement doesn’t seem to account for all the improvement in near focus that patients get with the lens.
Paul Dougherty, MD, one of the lens’s chief investigators, says the improved near vision is probably the result of a combination of three main factors. “The mechanism of this lens is likely more pseudo-accommodative, with a relationship between the pupil size, some induced higher-order aberrations, such as coma, which are part of the natural mechanism of near focusing; and some lens movement,” he says. “A smaller pupil leads to more depth of focus, so I think that’s clearly part of the mechanism with all lenses that are dubbed accommodating. However, if that were the only thing going on, then all monofocal acrylics would give reading vision, but they don’t. So it must be a combination of anterior movement, pupil size and induced higher-order aberrations that help near focus.”
In the Tetraflex data that was submitted to the FDA, there were 606 eyes of 351 patients analyzed for safety and 229 cases of bilateral implantations analyzed for efficacy using binocular testing. In the latter, 75 percent saw 20/20 or better uncorrected at distance postop, and all saw 20/40 or better. At intermediate distances, 20 percent saw 20/20 or better and 86 percent saw 20/40 or better. At near uncorrected, 81 percent read J6, which is the equivalent of stock quotes in the newspaper. When wearing distance correction but looking at near, 68 percent of the patients read J6, 86 percent read J8 (equal to print in a phone book) and 95 percent read J9 (newspaper print).
Dr. Dougherty thinks reading speed may be an even better measure of efficacy, however, since he says it’s a real-world use of near vision, ra-ther than “showing someone optotypes on a chart and seeing how far you can push him.” At one year, in a test of 239 Tetraflex patients and 96 controls implanted with a three-piece collamer monofocal lens, the Tetraflex patients had statistically significantly higher reading speeds at all print sizes from 20/25 to 20/80, Dr. Dougherty says. Seventy-five percent of the Tetraflex patients either never wore readers or wore them occasionally for small print or in dim light, vs. 46 percent of the control patients.
The study also looked at the amplitude of accommodation provided by the lens. At one year, 72 percent of the patients had 1 D or more of accommodation, 52 percent had 1.5 D or more and 31 percent had 2 D or more. “This is similar to what I have ob---served clinically,” avers Dr. Dougherty. “I find that the lens gets around 1.5 D of accommodation. If a prospective candidate were in my office, I would tell him that, if he decided to have the lens implanted, he’d get excellent distance and intermediate vision and good reading, but that it’s hard to tell how much reading vision he’d get. I would tell him that reading ability varies from one patient to another and that we don’t understand all the factors that influence who’s going to get the best reading vision.”
 AMO/Visiogen Synchrony
AMO/Visiogen Synchrony
The Synchrony is a silicone, one-piece, foldable IOL that makes use of a +32-D anterior optic and a posterior optic with a negative power value that’s chosen preoperatively. The two halves are connected via a spring mechanism. With the ciliary body at rest, the optics remain in proximity to each other and the eye is set for viewing distant objects. The theory of the lens holds that, when the ciliary body subsequently contracts, tension on the capsular bag and zonules is released and the front lens moves anteriorly, shifting the focus to intermediate and near distances. More than 300 patients have undergone bilateral Synchrony implantation in the U.S. FDA trial of the lens, and 1,300 have been implanted worldwide. The company’s pre-market approval application is still under review by the FDA.
Though the company won’t comment on the data currently being reviewed by the FDA, the lens has been studied elsewhere. In a recent prospective case series from Bogota, Colombia, researchers analyzed the reading ability of Synchrony patients over a two-year period. The physicians used standardized reading charts that were based on the MNRead charts developed at the University of Minnesota for testing reading ability in both normal and low-vision patients. The testing was performed with distance correction in place and without any near add at a distance of 40 cm. The test’s sentences contained print sizes ranging from 1.0 (equivalent to a newspaper subheadline) to 0.0 logMAR (20/20 vision, a little smaller than the size of reference footnotes). At two years, the patients had statistically significantly better reading speed than they had previously, with significant differences at print sizes from 0.3 (newspaper print) to 0.1 logMAR (footnotes) (p<0.01). The average reading acuity was also statistically significantly better, at 0.07 logMAR (a little better than 20/25 Snellen) vs. 0.15 logMAR (a little worse than 20/25) (p<0.01). The researchers didn’t find a difference in reading speed at 0.4 logMAR (newspaper print or 20/50) between one and two years.1
In a study presented at the 2007 meeting of the American Society of Cataract and Refractive Surgery by Colombian surgeon Ivan Ossma-Gomez, 46 eyes of 23 patients received bilateral Synchrony implantation. Postop, all eyes were within ±1 D of emmetropia, and the average distance acuity was -0.022 logMAR (a little better than 20/20), the average distance-corrected intermediate acuity was 0.027 (a little below 20/20) and the average distance-corrected near acuity was 0.114 (a little less than 20/25). The researchers found that reading speed averaged 173 words per minute (range: 141 to 193) at six months.
The medical monitor of the Synchrony U.S. trial, David Chang, MD, of Los Altos, Calif., presented a study at the 2010 ASCRS meeting examining the lens’s ability to move in the eye. “Although the testing is difficult to perform, ultrasound biomicroscopy imaging has been used to show optic movement with accommodative effort in a number of eyes,” Dr. Chang says. “It’s also possible to document an objective change in refraction using wavefront analysis with the iTrace system. At last year’s ASCRS meeting, I presented three-year results using these two objective studies from five selected patients implanted outside the U.S. Although it was a small cohort, these patients had subjective evidence of accommodation that correlated nicely with objective evidence using the two different technologies.”
 |
Dr. Chang says the lens may lend itself to an implantation that involves the use of a femtosecond laser, since the capsulorhexis size and placement are crucial. “Because the IOL design permits forward movement of the anterior optic, that optic must be completely overlapped by the capsulorhexis to prevent forward dislocation,” he says. “Although all eyes have been implanted through a manually created capsulorhexis, one can envision advantages of a precisely sized and centered capsulotomy created with a femtosecond laser.”
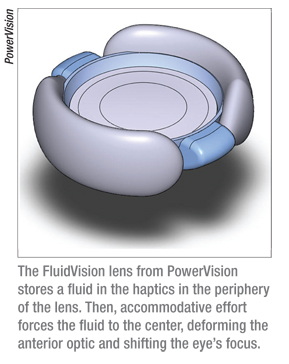
PowerVision’s FluidVision Lens
This lens, still in the early clinical stages according to company founder and chief business officer Matthew Frinzi, relies on a shape change of the anterior optic in order to create “dramatic” optical power shifts in the eye.
The theory behind the lens design is that fluid is stored in the haptics in the periphery of the IOL and then moved to a centralized membrane by the ciliary force generated during accommodative effort. This accumulation of fluid deforms the anterior optic which brings the focus to near. The optic diameter is 6 mm.
 The initial studies with the lens had surgeons implanting it in one eye of patients through large 8- or 9-mm incisions. “These studies helped us better understand sizing issues and the impact of capsular changes on the device,” explains Mr. Frinzi. “The distance visual acuities have been acceptable and the accommodation was greater than 5 D in six patients on subjective tests using push-up and push-down testing methods. Our fundamental goals in these early clinical tests were to determine if the lens maintained stability in the eye, delivered acceptable distance vision and provided at least 5 D of accommodation. These goals were met with this initial set of patients. The next group of patients will be implanted through a much smaller incision which we believe will enhance visual outcomes.”
The initial studies with the lens had surgeons implanting it in one eye of patients through large 8- or 9-mm incisions. “These studies helped us better understand sizing issues and the impact of capsular changes on the device,” explains Mr. Frinzi. “The distance visual acuities have been acceptable and the accommodation was greater than 5 D in six patients on subjective tests using push-up and push-down testing methods. Our fundamental goals in these early clinical tests were to determine if the lens maintained stability in the eye, delivered acceptable distance vision and provided at least 5 D of accommodation. These goals were met with this initial set of patients. The next group of patients will be implanted through a much smaller incision which we believe will enhance visual outcomes.”
Mr. Frinzi says one of the company’s major design goals is for the FluidVision’s implantation process to be similar to current methods used to implant conventional IOLs. Naturally, that will involve using an incision smaller than 9 mm. To that end, the company is developing a novel proprietary delivery system that will enable the surgeon to safely implant the Fluid-Vision lens through a sub-5 mm incision. Powervision expects to discuss the delivery system in more detail at the ASCRS meeting in March of this year.
The NuLens DynaCurve
The DynaCurve (NuLens Ltd., Herzliya Pituah, Israel) is an out-of-the-bag IOL, based instead in the sulcus. The lens’s design involves poly(methyl methacrylate) haptics, a PMMA anterior lens that the company calls a “reference plane” that provides distance correction, a small chamber that contains a solid silicone gel, and a posteriorly situated piston with an aperture in the center. The haptics are secured by internal scleral fixation to the sulcus without sutures. As described in one of the lens’s initial studies, the chamber containing the flexible gel is in a fixed position in the eye. The piston, moved by ciliary muscle force, presses the gel through a round hole to form a bulge that functions as a lens that focuses an image on the retina.2 The initial design needed a 9-mm incision.
“The change of the gel membrane provides a mean of 8 D of accommodation in our tests using pilocarpine,” says NuLens investigator Jorge Alio, MD, PhD, of Alicante, Spain. Non-pilocarpine-stimulated patients get 5 to 6 D of accommodation. “There’s also a new design for the lens that includes a platform and a lens,” he says. “The new platform creates the support for the lens to function, and allows the use of an incision that’s 3.5 to 4 mm. This was a major design factor, since the lens used to need a 9-mm incision. This smaller incision is important for modern cataract surgery.”
 |
To implant the correct power, Dr. Alio performs high-frequency ultrasound imaging to determine the eye’s sulcus-to-sulcus distance, then sends that data to the company. “The lens power is then calculated for the patient by NuLens,” he explains. “So, the lens is customized for each eye in that way.”
Dr. Alio says the company hopes to commercialize the lens for monocular implantation in Europe by the end of 2011. “The company is looking for a mature product with very clear indications on how to calculate its power and use it correctly,” he says.
Dr. Dougherty is a consultant for Lenstec and Dr. Alio is a clinical investigator for NuLens.
Dr. Chang is a consultant for AMO, although his consulting fees are donated to Project Vision and the Himalayan Cataract Project.
1. Bohórquez V, Alarcon R. Long-term reading performance in patients with bilateral dual-optic accommodating intraocular lenses. J Cataract Refract Surg 2010;3611:1880-6.
2. Alio JL, Ben-nun J, Rodriguez-Prats J, Plaza AB. Visual and accommodative outcomes one year after implantation of an accommodating intraocular lens based on a new concept. J Cataract Refract Surg 2009;35:10:1671-78.



