When deciding whether a patient is a good candidate for laser phototherapeutic keratectomy, I ask myself two questions. Question 1: Does the patient have corneal pathology in the anterior one-third of the cornea? (Ideally, the pathology is in the top 10 percent to 20 percent; PTK has been approved to treat up to one-third of the cornea, but one-third is getting pretty deep for PTK.) Question 2: Does the corneal pathology account for the patient’s visual and/or discomfort symptoms? In other words, if I fix the cornea, will I be helping the patient?
After determining that a patient is a good candidate for PTK, I classify his or her pathology into one of three categories: elevated lesions, stromal lesions and epithelial or recurrent erosions.
Elevated Lesions
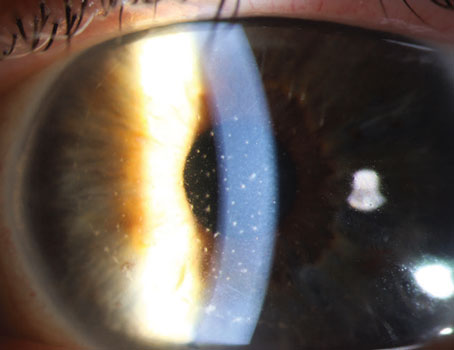
The most common elevated lesion I see is Salzmann’s nodular degeneration. These patients have nodules that are usually located in the periphery of the cornea. If they are mild, patients are usually asymptomatic. If they are moderate, they can cause some discomfort and a change in vision. If they are large or central, they can severely affect vision. If I am considering a patient for PTK treatment, he or she has already tried medical treatment and possibly also contact lenses.
For these patients, my preference is to bring them to the laser suite and debulk the nodules with a blade. I try to peel it off as well as I can mechanically with a blade such as a #15. Often, you can achieve a reasonably smooth plane between the nodule and the rest of the cornea. If I get a smooth underlying surface, then I will usually treat it with a little bit of PTK just to smooth it out a little bit more. It’s often just 5 to 10 µm of laser ablation. I may or may not use a masking agent, but I typically don’t because the underlying surface is pretty smooth. There is usually some haze, and my goal is not to get rid of all that haze.
Some patients may not achieve a smooth surface after debulking the nodule. Those patients require a lot more PTK treatment. I will set the laser to a relatively small spot size—1 to 4 mm diameter, depending on the size of the nodules.
I’ll use some masking agent to fill in the valleys. Basically, I will “paint” the nodules with the laser until I have shaved them down to be on a level playing field with the rest of the cornea. While it sounds fairly simple, it’s actually rather tricky. It’s hard to tell exactly how much you are doing, and it’s difficult to get a nice smooth surface, but that’s my goal.
| ||||||
I will usually start with smaller spot sizes, and then I will go up to a 4- to 6.5-mm diameter spot size and smooth out the entire area with bigger spot sizes. When I am treating Salzmann’s nodules, I usually use mitomycin-C 0.02% on an 8-mm sponge for 60 seconds once the debulking and the laser treatment have been completed. I’ll then irrigate it with 30 cc of saline. In my experience, using mitomycin-C decreases the chance of recurrent scar tissue and recurrent nodules. It doesn’t eliminate it, but it decreases it.
| ||||||
Stromal Lesions
For patients with stromal lesions, if there is significant thinning of the cornea or if the opacity goes rather deep in the cornea, then they are not good candidates for PTK. The best candidates are patients with stromal dystrophies, for example, granular dystrophy, lattice dystrophy, and Reis-Buckler’s dystrophy. These patients respond well.
If the epithelium is smooth, I typically take a large spot size (with the Visx laser, the PTK mode will go out to a 6.5-mm diameter circle), and I’ll do a central, transepithelial ablation. I center the light right on the pupil, and without scraping anything off, I will start ablating through the epithelium and into the stroma. Preoperatively, I get an idea of the depth of the pathology through a combination of the slit-lamp exam and ultrasound pachymetry or Scheimpflug imaging.
As an example, if the pachymetry is 500 µm and the pathology I want to remove is about 20 percent of the cornea, then I’m thinking I have to remove about 100 µm, which includes the epithelium. I will set the laser to about two-thirds of that, so to about 66 µm. I’ll do the transepithelial ablation, and I will stop at around 66 µm and then reassess. Under the laser microscope or, ideally, at a slit lamp, I put some saline in, and I get an idea of how much opacity is left there. If more needs to be removed, I bring the patient back to the laser and remove another 10 or 15 µm. Then, I reassess. I may repeat this “laser and check” process a few times during one procedure.
The goal is a much clearer and smoother cornea, but not necessarily a crystal clear cornea. If you remove the bulk of the opacity, you can improve the patient’s symptoms significantly and decrease the chance of side effects and complications. The two main complications that I’m concerned about are corneal scarring and significant corneal flattening. The deeper you go, the more corneal flattening and induced hyperopia you’ll get.
The key is that you don’t have to get all the opacity because sometimes if you go to 60 µm, you can get rid of 80 percent of the opacity, but to get rid of the last 20 percent, you need to go another 60 µm. If you go the other 60 µm, you have hugely increased your risk of problems. You may have made the cornea a little bit clearer, but the patient will be much less happy with the results. If I’ve gone deep, sometimes, I use mitomycin in these patients to decrease the chance of scarring.
For patients with a stromal opacity and an irregular epithelium, I usually remove the epithelium mechanically with a blade and then do a stromal ablation. You then have to subtract the epithelial thickness, usually about 45 µm, from your calculations. Generally, I would like these patients to end up plano postoperatively. But sometimes, I have to ablate rather deep to remove the bulk of the opacity. In such cases, if I’m afraid of inducing hyperopia, I will remove the epithelium from the outside edge of the laser treatment. My typical laser treatment is about 6.5 mm in diameter, so I will remove the epithelium from the outside 1 or 2 mm peripheral to that. Then, I will take a 2-mm diameter spot, and I will then straddle my original ablation. I’ll just laser around my original 6.5-mm diameter circle, so it’s like I am deepening my peripheral ablation and smoothing out that ledge I created.
There is no absolute, but I will do it for a total of usually 120 to 200 µm, going evenly around the circle. This is a very nonscientific way of decreasing the amount of induced hyperopia, but it seems to work.
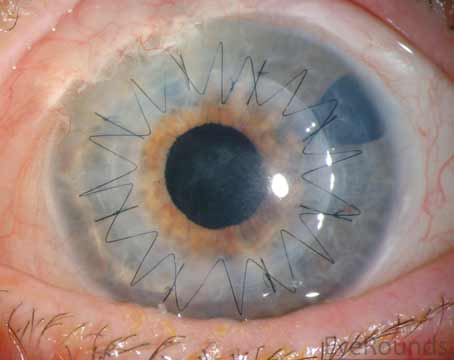
Epithelial or Recurrent Erosions
|
Usually, I treat recurrent erosions in the office with a diamond burr polishing treatment, but some patients fail the diamond burr and require PTK or decline the diamond burr treatment and prefer PTK. For those patients, I remove all the loose epithelium under the laser, and then I treat Bowman’s layer with a 5-µm treatment. However, the treatment should be uniform and should not split the visual axis. I do a 5-µm treatment centered on the pupil; I take my 6.5-mm diameter spot, and I center on the pupil after taking the epithelium off.
Then, assuming I have areas outside the central 6.5-mm diameter area I just treated—which I usually will because I am usually going out to approximately 10 mm—I will take a little 6.5-mm blocker (you can create this using a 6.5-mm trephine to cut a sponge or piece of paper). I will put that on my central cornea to basically protect the cornea I just treated. Then, I will change my spot size to 4 mm, and I will treat the area of recurrent erosion with 4-mm spots for just 5-µm each. I will center my spot at 3 o’clock. I will move the joystick and repeat until all areas from which the epithelium has been removed have been treated but not doubly treated. You don’t want to double treat some areas and not treat other areas. This is especially important in the center, which is why I place the blocker in the center.
Postoperatively, I typically use a bandage contact lens. Usually, I use an Acuvue Oasys (8.8, 14.0, plano), and I treat with topical antibiotics, such as a fluoroquinolone, four times a day. I also have patients use preservative-free tears frequently to keep the eye moist. I see patients one day postop and then three or four days after that. I remove the contact lens on day four or five postop, and I check on the epithelial defect. If it is healed, the patient continues the antibiotic for another day or two and then stops. If it is not well-healed, I place another bandage contact lens or use frequent antibiotic ointment.
When performing PTK, it is important for ophthalmologists to remember that these patients and these corneas are not as healthy as other laser refractive surgery patients. Healing problems are more common after PTK than they are after PRK. These patients need closer follow-up and more hand-holding than PRK patients. REVIEW
Dr. Rapuano is in practice at Wills Eye Institute, where he is the chief of the Cornea Service and co-director of the Refractive Surgery Department.