In any surgery, the goal should be to perform the least invasive procedure to repair the pathology and to avoid intraoperative and postoperative complications. In this article, I’ll review the current methods of rhegmatogenous retinal detachment repair, which include pneumatic retinopexy, scleral buckling and pars plana vitrectomy, and I’ll discuss the University of British Columbia approach to detachment surgery.
I’ve been involved in the training of 60 vitreoretinal fellows, including 29 from the United States, 11 from Canada and 12 from Australia. By teaching all three methods in our vitreoretinal fellowship, we ensure that our graduate surgeons will be well equipped to address the many varieties of detachments with the appropriate procedure and achieve the best anatomic and visual results.
The UBC Serial Approach
In our fellowship training program, we teach a serial approach to the repair of RRD. We start by teaching the indications and benefits of the least invasive procedures, i.e., PnR and SB, and proceed with the indications and benefits of the more invasive PPV surgery.
The development of small-gauge vitrectomy units with high-speed cutters, wide-angle viewing systems, the use of intraocular gases SF6 and C3F8 and perfluorocarbon liquid has revolutionized the repair of RRD and led to the misconception that PnR and SB surgery are no longer necessary in the management of RRD.
 |
Many fellowship training programs in the United States, Europe and Australia no longer teach PnR and SB surgery, despite the fact that studies have shown that the anatomic and visual results of these procedures are better than PPV surgery, especially in young, phakic patients.1,2 These programs teach only PPV surgery in the management of RRD and accept the complication of cataract formation within one to two years and its sequelae.3,4,5
I feel strongly that teaching PnR and SB surgery should be an integral part of any vitreoretinal fellowship training program. In this article, I’ll outline the indications and techniques of PnR, SB and PPV surgery and discuss the complications of PPV surgery in phakic patients.
Lens Status and Age of Patients Who Present With RRD
It’s important for the vitreoretinal surgeon to realize that the majority of patients who present with retinal detachments are phakic. The Netherlands study of 2,998 cases revealed that a full two-thirds, or 66.5 percent, of patients who presented with retinal detachments were phakic. It also demonstrated that the age of patients with detachments ranged from 55 to 59 years.6 Since PnR and SB surgery don’t result in cataract formation, they should be considered as the first options in the repair of RRD.
UBC Serial Approach to RRD Repair
1. Pneumatic retinopexy. PnR is the least invasive surgery and is especially suitable for phakic patients. It’s performed using topical anesthesia in the office or in an outpatient setting. The procedure usually takes between 15 and 20 minutes. Approximately 40 percent of patients who present with RRD can be managed with PnR surgery.7
Indications. RRDs that involve the superior retina—i.e., between the 8 and 4 o’clock positions—have one to two breaks no farther apart than one clock hour and have no evidence of fixed retinal folds, holes with rolled edges or vitreous hemorrhage are especially suitable for PnR surgery.
Mechanism of repair. The buoyancy and surface tension of the gas bubble closes the retinal tear and allows the pigment epithelial layer to absorb the subretinal fluid. This method of repair allows the neurosensory retina to slowly reattach to the pigment epithelial layer, resulting in a high-integrity retinal attachment. (This concept will be discussed shortly.)
Preoperative discussion. Prior to performing the pneumatic procedure, we inform our phakic patients that there’s a 70- to 75-percent chance, and our pseudophakic patients that there’s a 60- to 65-percent chance, of surgical success. We also advise them that in phakic patients SB—and PPV surgery in pseudophakic patients—can also be used to repair the RRD. However, these procedures require hospital admission and are performed in the operating room.
Most patients will choose the first option of PnR. For those patients who choose not to proceed with an initial PnR surgery, we would schedule them for SB or PPV procedures. We would also advise against PnR surgery if the patient has to fly within seven to 10 days after the procedure.
Technique. First, perform a preoperative dilated fundus examination to ensure that the detachment meets the indications for PnR surgery.
On the day of surgery, administer topical or subconjunctival anesthesia in the office or outpatient clinic. Next, perform cryopexy of the retinal tear (postoperative laser treatment is also an option). Create an anterior chamber paracentesis to release 0.2 to 0.3 cc of aqueous fluid. After the paracentesis is created, inject 0.5 to 0.6 cc of SF6 gas through the pars plana into the vitreous cavity. Position the patient so that the gas bubble will tamponade the retinal tear.
Result. As noted earlier, in phakic patients, we anticipate a 70- to 75-percent success rate. In pseudophakic patients, we anticipate a 60- to 65-percent success rate.8,9
Complications. Failure to flatten the retina occurs in approximately 25 to 35 percent of patients. Causes of failure include the inability of the patient to position properly, the development of a new retinal tear as the gas bubble expands and residual persistent traction on the original tear after the gas bubble resorbs. After these initial failures, a subsequent SB procedure in a phakic patient would be performed with an anticipated reattachment rate of 92 to 94 percent. In the 6 to 8 percent of SB failures in phakic patients, a subsequent PPV would result in a final reattachment rate of 98 to 99 percent. In pseudophakic patients who don’t respond to a PnR, a subsequent PPV would also result in a final reattachment rate of 98 to 99 percent.
It’s important to note that an initial PnR failure has no adverse anatomic or visual effects on subsequent SB or PPV surgery.
Comments. The PIVOT Study by Roxane J. Hillier, MD, and her colleagues compared PnR surgery with PPV in the management of 176 phakic patients. At 12 months, a primary anatomic success rate was achieved in 80.8 percent of patients undergoing PnR versus 93.2 percent of PPV patients (p=0.045). Final anatomic success was 98.7 percent in the PnR group and 98.6 percent in the PPV group. Final visual acuity after one year was 20/40 in 90.3 percent of the PnR group compared to 75.3 percent in the PPV group. More importantly, 65 percent of phakic patients in the PPV group, as opposed to 16 percent in the PnR group, underwent cataract surgery within 12 months (p<0.001).2
A more recent, retrospective study by Rajeev Muni, MD, and colleagues involving 238 cases used fundus autofluorescence images to detect retinal vessel displacement in patients who had undergone PnR and PPV surgery. Retinal vessel displacement occurred in only 15 percent of patients undergoing PnR, compared to 42 percent of patients undergoing PPV.10
This study may explain the better postoperative vision in non-drainage PnR surgery. In PnR surgery a higher-integrity retinal reattachment is achieved by the retina being re-apposed as close as possible to the original location with no retinal vessel printing shown on fundus autofluorescence imaging. This presumably indicates alignment of the photoreceptors closer to their specific retinal pigment epithelial cell and therefore better final visual acuity.
2. Scleral Buckling. Scleral buckling surgery is the ideal procedure for phakic patients. Two-thirds of patients who present with RRD are phakic with an average age between 55 and 59 years.
SB surgery is an external procedure performed in the operating room using retrobulbar anesthesia. Since local retrobulbar anesthesia is used, the globe is made more accessible for placement of the silicone explant and the scleral sutures. The patient doesn’t feel any pain during this procedure, which takes approximately 30 to 40 minutes.
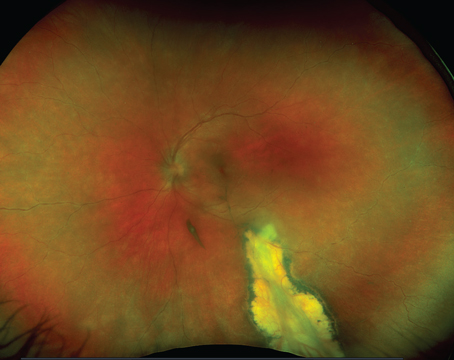
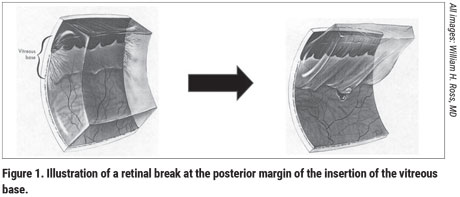
A surgical innovation: The 5-mm encircling silicone band. The vast majority of retinal tears are 1 to 3 mm in size and occur at the posterior margin of the insertion of the vitreous base, i.e., 3 to 4 mm from the ora serrata (Figure 1). Therefore, a scleral buckle that covers 5 to 7 mm of peripheral retina will close most retinal tears.
In 2003, I developed a 5-mm-wide, 0.75-mm-high encircling band to manage RRD (Ross 5; MIRA Inc., Uxbridge, Mass.) and its compatible sleeve (Ross 75R; MIRA Inc.). The advantages of this explant are as follows: It’s thin and therefore easy to place around the globe for 360 degrees under local anesthesia. Because of its thinness, it doesn’t disturb extraocular muscle function and there’s no postoperative diplopia. There’s little, if any, induction of myopia since the band is enclosed—not tightened—by a silicone sleeve (Ross 75R). There’s little chance of infection or rejection since the band is well-covered by Tenon’s capsule and conjunctiva at the end of the procedure. Postoperatively, there’s little, if any, pain.
The encircling explant will close the original tear(s), relieve vitreoretinal traction for 360 degrees and prevent the formation of new retinal tears, which could lead to redetachment. Because of these properties, the Ross 5 band has become very popular as an explant in SB surgery in Canada, the United States, Europe and Australia.
Indications. The indications for SB surgery are as follows:
- Patients who are suitable but refuse PnR surgery. This could be due to an inability or unwillingness to position for three to four days following gas bubble injection; anxiety; or systemic conditions such as obesity or arthritis.
- Patients with superior retinal breaks that are too far apart to be treated with a PnR procedure, e.g., breaks at the 10 o’clock and 2 o’clock positions.
- Failed PnRs, due to the development of new inferior retinal breaks.
- Inferior retinal detachments, especially in high myopes, which represent 35 percent of detachments.11 These detachments are often secondary to retinal breaks at the lateral or posterior margins of lattice degeneration.
- Detachments secondary to traumatic retinal dialysis. These types of detachments occur mainly in young males as a result of trauma. In 1981, I reported on 50 cases of traumatic retinal dialysis managed with SB surgery with a 98-percent success rate.12,13
- Retinoschisis retinal detachments. In these cases small inner retinal breaks near the vitreous base develop as a result of an acute posterior vitreous detachment. These anterior inner-layer breaks allow liquid vitreous to gain entry into the retinoschisis cavity, pass through the outer retinal breaks and lead to neurosensory detachments. An encircling 5-mm band will close the small anterior retinal breaks and repair the detachment.
Mechanism of repair. The silicone band indents the sclera and approximates the retinal tear to the pigment epithelial cells. This indentation results in a relief of vitreous traction on the retinal tear and allows the retinal pigment epithelial layer to absorb the subretinal fluid. External drainage of subretinal fluid isn’t necessary. If the 5-mm explant has been properly positioned to close the retinal tear, the fluid on the buckle and posterior to it will slowly resorb over two to three days.
Technique. SB surgery is an external procedure, except for anterior chamber paracentesis and possible drainage of subretinal fluid. In approximately 60 to 70 percent of cases, SB surgery can be carried out using an encircling band without drainage of subretinal fluid.
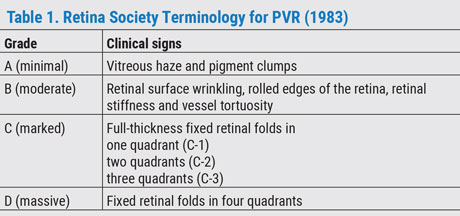 |
Prior to performing SB surgery, a peripheral retinal examination with 360-degree scleral depression must be carried out to identify all retinal tears and to identify and grade possible proliferative vitreoretinopathy (PVR) (Table).
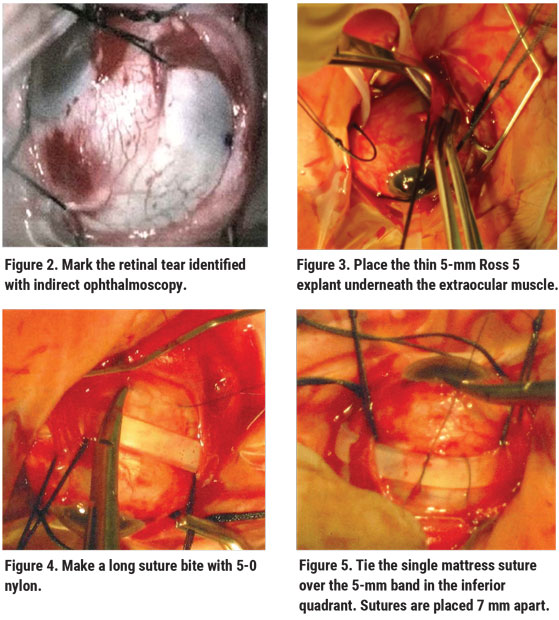
On the day of surgery, administer retrobulbar anesthesia. Open the conjunctiva for 360 degrees and hook the recti muscles with 3-0 silk sutures. Perform indirect ophthalmoscopy to identify and mark all retinal breaks (Figure 2), and then perform cryopexy of retinal tear(s). (Postoperative laser can also be used.)
Once the breaks are treated, place the encircling Ross 5 explant beneath the recti muscles for 360 degrees (Figure 3). Place a single 5-0 nylon mattress suture in each of the two inferior quadrants. These sutures are spaced 7 mm apart to cover the 5-mm band. The anterior scleral suture is placed 2 mm posterior to the ora serrata (line of muscle insertion) and the posterior suture is placed 7 mm posterior to the anterior bite. If the retinal tear is found to be more posterior, then the sutures are retro-placed 7 mm apart. We teach fellows to use long suture bites with 5-0 nylon so that when the suture is tied there’s less shredding of the sclera (Figure 4). Tie the 5-0 nylon mattress sutures in the two inferior quadrants (Figure 5).
 |
Next, perform an anterior chamber paracentesis. Place and tie a single 5-0 nylon mattress suture in each of the two superior quadrants. Use 2 to 3 mm of the Ross 75R silicone sleeve to enclose—not tighten—the explant to avoid myopia (Figure 6) and remove the 3-0 silk sutures.
Finally, close Tenon’s capsule and conjunctiva with 7-0 vicryl or 6-0 plain gut, and perform indirect ophthalmoscopy to check for central retinal artery pulsations. If indirect ophthalmoscopy reveals a lack of pulsations in the central retinal artery, perform a second anterior chamber paracentesis.
 |
We prefer non-drainage SB surgery. As noted earlier, this applies to approximately 60 to 70 percent of our phakic retinal detachments. As in PnR procedures, this approach results in a slower re-apposition of the neurosensory retina to the pigment epithelial layer and a final, better postoperative visual acuity due to a higher-integrity retinal reattachment.
Patients who present with phakic detachments and associated PVR grades B, C-1 or C-2—i.e., retinal tears with rolled edges or fixed folds in one or two quadrants—are also candidates for SB surgery. For these detachments we can use a 5-mm encircling band or a 6- to 7-mm biconvex solid silicone explant. If a segmental buckle is used, two mattress sutures are placed 7 to 8 mm apart over the solid silicone explant in each quadrant. We then place a 2-mm encircling band through the groove in the explant, pass it around the globe and tie it with one mattress suture in each quadrant. Subretinal fluid is drained beneath the scleral explant and away from any retinal tears. This is followed by the injection of filtered air or balanced salt solution to maintain globe volume and prevent postoperative myopia. Again, just as in the other procedure, the 2-mm encircling band is enclosed in a sleeve without tightening the ends of the band to prevent myopia.
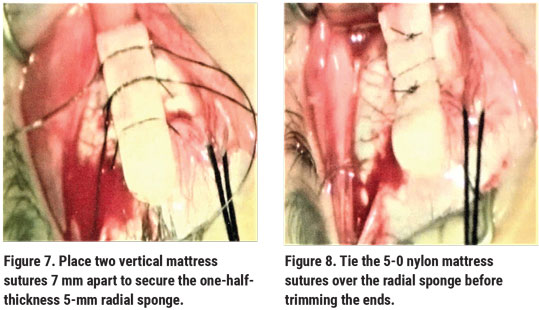 |
Patients with a posterior equatorial retinal break. These cases are managed differently. Radial sponges are especially suitable for closing the posterior break in these cases. Using two vertical mattress sutures, the radial sponge is sutured in the same meridian as the posterior equatorial retinal tear (Figures 7 and 8), supporting the tear and closing it nicely. There’s no fish-mouthing of the retinal break, as would occur if a circumferential element was used to close the posterior retinal break. We use half-thickness 5- to 7-mm radial sponges with tapered ends. The sutures are placed 7 to 9 mm apart, depending on the size of the retinal tear. The sponge is then covered completely with Tenon’s capsule and conjunctiva. If the sponge is well-covered, the risk of infection or rejection is very small.
In 1977, I reported on 100 cases of radial sponges used in retinal detachment surgery. The success rate was 94 percent. In two cases, there was rejection of the radial sponge.14
Complications. SB surgery has two major complications. The first is a failure of reattachment due to PVR grades C-1 to C-3. (Subsequent PPV surgery would result in a reattachment rate of 98 to 99 percent.) Second, subretinal hemorrhage or retinal incarceration can occur following drainage of subretinal fluid.
Comments. In my experience, the anatomic and visual results of SB surgery are equal to or better than PPV in the repair of phakic detachments. A prospective, randomized, multicenter clinical study reviewed the management of RRD in phakic patients and reported single-operation success rates of 63.6 percent and 63.8 percent, respectively, for SB and PPV in phakic detachments.1 In our hands we anticipate a single operation success rate of more than 90 percent for both SB and PPV surgeries.
We recently reviewed the management of RRD in 100 phakic patients in our department who underwent SB surgery without drainage of subretinal fluid.15 In 67 patients, an encircling 5-mm Ross band was used. In 19 cases a 6-mm silicone explant with a 2-mm encircling band was used, and in 12 cases, a radial sponge was used. The primary anatomic success rate was 97 percent and the final success rate was 100 percent, following secondary PPV surgery.
In combined macula-on and macula-off detachments, the average postoperative vision was 20/40. In the macula-off detachments, 60 percent of patients regained 20/50 or better vision and 29 percent achieved 20/30 or better vision.
In reviewing the literature of macula-off detachments, a visual recovery of 20/50 or better is only obtained in 40 percent of cases.16 We feel strongly that our higher final vision was due to the high-integrity retinal reattachment resulting from slower re-apposition of the neurosensory retina to the pigment epithelial layer.
3. Pars plana vitrectomy. In our department, we perform primary PPV in approximately 30 percent of our RRD cases.
Indications. These include:
- phakic elderly patients with moderate cataracts;
- phakic patients who present with giant retinal tears;
- phakic and pseudophakic patients with vitreous hemorrhage that obscures a view of the peripheral retina;
- pseudophakic patients with tears not suitable for PnR;
- pseudophakic patients with mild PVR, i.e., grades A, B; and
- failed PnR procedures.
Mechanism of repair. The retina is reattached by removing the vitreous with high-speed cutters, draining subretinal fluid through a peripheral break, flattening the retina with an air-fluid exchange, and lasering the retinal tears and the peripheral retina, followed by gas-air exchange.
Technique. First, a core vitrectomy is performed and the remaining vitreous is then stained with Kenalog or Triesence. This residual vitreous is then removed with peripheral shaving, aided by scleral depression, and the retinal tears are marked with endodiathermy. At this point, you can use microforceps to strip membranes from the retina surfaces, if necessary.
Then, using active suction, subretinal fluid is drained through an existing peripheral retinal tear as an air-fluid exchange is carried out. This results in flattening of the retina. Endolaser is then applied around the retinal tear(s), and three rows of laser are applied to the peripheral retina for 360 degrees. Finally, SF6 or C3F8 air exchange is performed.
Although perfluorocarbon liquid can also be used to flatten the retina from the posterior pole to the ora serrata, this is not our preferred technique.
 |
4. Combined vitrectomy and scleral buckling procedures. This approach is used in approximately 20 percent of our RRDs.
Indications. These include:
- phakic patients with severe PVR grades C-2, C-3 and D—i.e., fixed folds in three or more quadrants;
- phakic patients with vitreous hemorrhage that obscures a view of the peripheral retina;
- giant retinal tears where the buckle is used to support the lateral horns of the tear; and
- failed SB procedures. In these cases we apply three rows of laser on the buckle for 360 degrees at the end of the procedure.
Rationale. The encircling 5-mm band is placed around the globe to relieve vitreous traction on the peripheral retina before proceeding with PPV.
Technique. Place the 5-mm band around the globe with one mattress suture in each quadrant. Enclose the band in a silicone sleeve. Proceed with PPV as outlined above. Place three rows of laser photocoagulation on the buckle at the end of the procedure.
Recent studies have shown that a combined SB and PPV surgery results in a higher anatomic success rate than PPV surgery alone.17
Complications. The complications of vitrectomy surgery in phakic patients include:
- Progression of lens opacities, requiring cataract surgery within one to two years.
- Loss of accommodation following cataract surgery.
- In myopic patients (35 percent of RRD),16 anisometropia following cataract surgery. This would require the patient to wear a contact lens or undergo clear lens extraction in the fellow eye.
- An increased stimulus for postoperative PVR. PPV is an invasion of the vitreous.
- Restriction of air travel due to gas expansion and elevated IOP following PPV surgery.
In conclusion, approximately 50 percent of all patients who present with RRD meet the criteria and can be successfully repaired with PnR or SB surgery. I strongly believe that these procedures are the treatments of choice to manage RRD, especially in phakic patients. Primary PnR and SB surgery produce equal or better anatomic and visual results compared to PPV surgery, without the complication of cataract formation and its sequelae. REVIEW
Dr. Ross is a clinical professor of ophthalmology and the co-director of the vitreoretinal fellowship program at the University of British Columbia, Vancouver. He has no financial disclosures related to any product mentioned in the article.
1. Heinmann H, Bartz-Schmid KU, Bornfeld N, et al. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment: A prospective randomized multicenter clinical study. Ophthalmol 2007;114:4:2142-54.
2. Hillier RJ, Felfeli T, Berger AR, et al. The pneumatic retinopexy versus vitrectomy for the management of primary rhegmatogenous retinal detachment outcomes randomized trial (PIVOT). Ophthalmol 2019;126:4:531-9.
3. D’amico DJ. Different preferences between United States and European vitreoretinal surgeons: Personal observations. Curr Opin Ophthalmol 2016;27:3:196-200.
4. Hwang JC. Regional practice patterns for retinal detachment repair in the United States. Am J Ophthalmol 2012;153:1125-8.
5. Jackson TL, Donachie PHJ, Sallam A. et al. United Kingdom National Ophthalmology Database Study of vitreoretinal surgery: Report 3, retinal detachment. Ophthalmol 2014;121:643-8.
6. Van de Put M, Hooymans J, Los L, et al. The incidence of rhegmatogenous retinal detachment in the Netherlands. Ophthalmol 2013; 120:3:616-22.
7. Brinton DA and Wilkinson CP. Pneumatic retinopexy and alternative retinal detachment techniques. In: Ryan SJ, ed. Retina, vol. 3. St. Louis: Mosby, 2001:2047-62.
8. Hilton GF and Grizzard WS. Pneumatic retinopexy: A two-step outpatient operation without conjunctival incision. Ophthalmology 1986;93:5:626-41.
9. Tornambe PE, Hilton GF, Brinton DA, et al. Pneumatic retinopexy: A two-year follow-up study of the multicenter clinical trial comparing pneumatic retinopexy with scleral buckling. Ophthalmol 1991; 98:1115-23.
10. Brosh K, Francisconi C, Qian J, et al. Retinal displacement following pneumatic retinopexy vs pars plana vitrectomy for rhegmatogenous retinal detachment. JAMA Ophthalmol 2020; 138:6:652-9.
11. Schepens C and Marden BA: Data on the natural history of retinal detachment. Am J Ophthalmol 1966;61:2:213-26.
12. Ross W. Traumatic retinal dialyses. Arch Ophthalmol 1981;99:1371-4.
13. Ross W. Retinal dialysis: Lack of evidence for a genetic cause. Can J Ophthalmol 1991;26:6:309-12.
14. Ross W. Radial sponges in retinal detachment surgery. Can J Ophthalmol 1977;12:4:268-74.
15. Ross W, et al. Modern techniques and indications for scleral buckling surgery. Submitted for publication.
16. Albert S, Smiddy WE, Venkatraman A and Feuer W. Visual recovery after scleral buckling procedure for retinal detachment. Ophthalmol 2006;113:10:1735-42.
17. Ryan EH, Joseph DP, Ryan CM, et al. Primary retinal detachment outcomes study: Methodology and overall outcomes—Primary retinal detachment outcomes study report number 1. Ophthalmol 2020;138:935-42.