Though multifocal IOLs are designed to work bilaterally to take advantage of binocular summation, many surgeons have had success mixing and matching different multifocal IOLs to increase the patient’s range of functional vision. Proponents say that mixing and matching complementary multifocals enables surgeons to take advantage of both IOLs’ best features while potentially minimizing common visual side effects such as glare, halo, reduced contrast sensitivity and reduced visual acuity in the intermediate and near ranges.
“Mix and match opens a range of different possibilities for treating patients with different visual expectations and different eye characteristics, such as subtle irregular corneas and large pupil sizes,” says César Vilar, MD, a cataract surgeon, medical researcher and medical director of the Hospital de Olhos Francisco Vilar in Teresina, Brazil.
Recently, the method has received new attention since good visual acuity at the intermediate range is more important than ever for computer and other technology-related tasks like reading on a tablet, and because more patients are demanding spectacle independence. In this article, cataract surgeons share their experience with the mix-and-match method and offer tips for choosing the best IOL combinations.
Mix and Match Beginnings
“Back when there were only monofocal intraocular lenses, inducing monovision (targeting plano in the dominant eye and a myopic target, such as -1.5 D or -2 D, in the non-dominant eye) was very common,” Dr. Vilar explains. “However, many patients complained about the lack of stereopsis.
“When the high-add bifocal intraocular lenses, such as the Alcon ReSTOR +4 D and the Tecnis ReZoom, were initially introduced, a large number of patients reported dissatisfaction due to poor quality of vision—mainly because of dysphotopsias,” he continues. “This discouraged many surgeons from implanting those lenses. The same thing happened with pseudo-accommodating lenses, because of the loss of function after capsule fibrosis. When low-add diffractive and EDOF lenses such as the ReSTOR +2.5 D and the Tecnis Symfony were introduced, surgeons promptly adopted these lenses and abandoned the high adds because patients reported fewer complaints. As a result, mix and match fell out of use.
“However, the low-add lenses didn’t provide enough near vision without the aid of spectacles for some patients,” he says. “This prompted surgeons to try placing a low-add EDOF in the dominant eye and a high-add EDOF in the non-dominant eye. This strategy delivered good to excellent results, and grew increasingly popular among surgeons.”
Kendall Donaldson, MD, MS, professor of clinical ophthalmology and medical director of Bascom Palmer Eye Institute at Plantation in Plantation, Florida, says we’re fortunate to have such a large range of lens options in 2020. “This allows us to customize cataract surgery to achieve the very best results for our patients,” she says. “Most lens manufacturers offer a variety of options providing various focal points and optical profiles.”
Complementary Combinations
“Surgeons around the world have differing opinions with regard to mixing and matching,” says Dr. Donaldson. “I think this is evidence that despite having achieved wonderful advances in the world of IOL technology, we still have no perfect lens that provides all focal points with optimal quality of vision and without side effects. There’s always a compromise between range and quality of vision.”
Dr. Vilar says that typical mix and match combinations used today include the Tecnis Symfony or the Tecnis multifocal ZKB00 (+2.75 D) in the dominant eye and the Tecnis ZMB00 (+4 D) or ZLB00 (+3.25 D) in the non-dominant eye; as well as the Zeiss AT LARA (an EDOF) in the dominant eye and a multifocal Zeiss AT LISA in the non-dominant eye (neither of which is approved in the United States). “You might also use the ReSTOR SN6AD1 (+3 D) in the non-dominant eye and the ReSTOR SV25T0 (+2.5 D),” he adds.
“Each lens manufacturer has generated a family of lenses with various focal points and optical profiles that work well together,” says Dr. Donaldson. “One excellent example of this synergy is the Johnson & Johnson family of lenses. I’ll often place a Synergy lens (EDOF) or Tecnis +2.75 D multifocal lens in the first eye and then evaluate the patient’s function and perception postoperatively. If the patient is 100-percent thrilled with the outcome, I’ll place the same lens in the second eye. However, if the patient wants more near vision, I may choose to increase the reading power with a Tecnis +3.25 D multifocal lens. Fortunately, these lenses are very complementary, and patients appreciate the increased range of vision at near distances when combining them.
“Similarly, Alcon has developed a family of ReSTOR lenses (+2.5 and +3 D) which also work very well together,” she says. For example, a ReSTOR +2.5 D in the dominant eye for good distance vision complements a ReSTOR +3 D in the nondominant eye for near vision. According to Dr. Donaldson, this combination can give a patient more freedom from reading glasses.
Since Alcon released its PanOptix lens last year, Dr. Donaldson says many surgeons who were using the Alcon ReSTOR lenses (+2.5 and +3 D) have switched to matched PanOptix lenses. “The PanOptix lens offers a broader range of vision when compared with the Alcon ReSTOR lenses, since it provides clear vision at three focal points: distance; intermediate; and near,” Dr. Donaldson says. “Since the release of this lens, I find that I’m matching lenses with a plano target more frequently within the Alcon platform. I think this is evidence that the technology has continued to improve. More patients are achieving good-quality vision with a broader range of vision, hence patients choose to proceed with the same lens that was placed in the first eye.”
 |
Combinations to Avoid
When mixing and matching different multifocal lenses, both Dr. Donaldson and Dr. Vilar emphasize the need to avoid creating a troubling level of anisometropia. One of the main critiques of the mix and match method is just that—that mixing different multifocal IOLs will result in patients comparing their eyes.
According to Dr. Donaldson, there’s more of a tendency for patients to become preoccupied with comparing the optical differences of each IOL when you mix different brands or lens families, such as a diffractive lens with a refractive lens. “I find that mixing and matching is most successful when lenses are mixed within the same family (manufacturer) because the optics are similar,” she notes. “Additionally, you should stick with one color of lens. Of note, Alcon lenses come in both clear and yellow (blue-blocking chromophore) versions.”
Bilateral vs. Mixed
“When compared to bilateral implantation of multifocal intraocular lenses, the mix-and-match method has been demonstrated to be superior in some respects by a number of studies,” says Dr. Vilar. He says the blended approach can increase a patient’s functional range of near vision. An Alcon study comparing 53 bilateral implantations of a +2.5-D multifocal and 50 blended implantations of a +2.5 and +3-D multifocal found both groups had similar visual results. The blended group had better, but not statistically significantly better, near visual acuity.1
 |
Compared to bilateral implantation of trifocal intraocular lenses, research has shown that both lens modalities produce good visual outcomes. The first reported comparison of multifocal mix-and-match implantation and bilateral trifocal implantation compared the AT LISA trifocal for bilateral implantation (n=25) and the ReSTOR for blended implantation (an intermediate add in the dominant eye and a near add in the nondominant eye) (n=30). It found that both methods provided good visual outcomes.2 (One of the researchers received a study grant from Alcon for the paper.) Both groups demonstrated excellent binocular near and distance vision, good visual function and similar low rates of dysphotopsias. The trifocal group had significantly better intermediate visual acuity from 2 m to 67 cm, corresponding to grocery shelves and car dashboards, and both groups had comparable visual acuity at distances from 60 cm to 40 cm, corresponding to computer or reading distance.
A prospective, nonrandomized, consecutive study comparing bilateral implantation of the PanOptix with blended implantation of the Tecnis Symfony and Tecnis ZMB00 multifocal included 40 eyes of 20 patients. Both groups achieved good acuity for distance, intermediate and near vision. The researchers say that the blended implantation group was superior for very near distances and for intermediate and long distances greater than or equal to -1.5 D of vergence. The bilateral trifocal group had superior uncorrected intermediate visual acuity at 60 cm and uncorrected near visual acuity at 40 cm.3
One purported advantage of the mix-and-match method is its ability to reduce unwanted photic phenomena through the use of complementary lenses. In a nonrandomized comparative study in Japan,4 researchers compared the visual outcomes of patients implanted bilaterally with a trifocal IOL and patients implanted with multifocals with a different near add in each eye (+3 D and +4 D). They found that the bilateral trifocal group demonstrated better distance and intermediate vision than the blended group (p≤0.0325), but both groups had comparable near visual acuity. While the trifocal group had significantly better contrast visual acuity and stereoacuity than the blended group, the incidence of halo symptoms tended to be worse in the trifocal group.
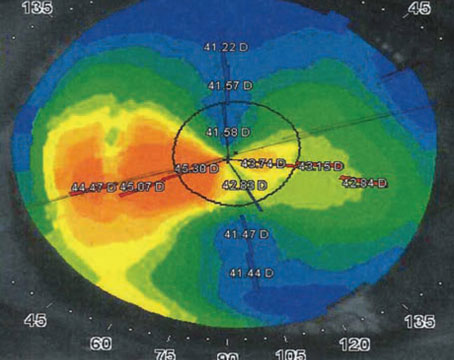
“Our group in Brasilia from CEORA published studies comparing the two different strategies,” says Dr. Vilar. “We analyzed VA outcomes, defocus curves and contrast sensitivity in 20 patients for either mix-and-match (ReSTOR +2.5 D and ReSTOR +3 D) or trifocal implantation in both eyes, and achieved similar results in both groups.”5 The study found that average preoperative CDVA was better in the blended group than in the trifocal group (0.15 versus 0.24 logMAR, Snellen: 20/28 versus 20/35; p=0.073), though the difference was not statistically significant. Defocus curves in both groups exhibited a trifocal pattern, but the trifocal demonstrated statistically significantly better visual acuity from -2 D to plano and at -3.5 D (Figure 1). Overall, the trifocal performed better and showed excellent visual acuity through a large interval of vergence (-0.1 and +0.1 logMAR [Snellen: 20/15 and 20/25] from -2.5 D to plano). Dr. Vilar says this suggests that bilateral trifocal implantation may have better tolerance of a hyperopic residual refractive error when compared to blended implantation.
Studies that employed questionnaires asking about subjective quality of vision didn’t find consistent differences between groups using mix-and-match approaches and groups that received bilateral implantation of trifocal lenses.6
Dr. Donaldson says that she’s found EDOF and diffractive multifocals work well together. “We did a study on mixing and matching EDOF
lenses with the Tecnis +3.25 D a couple of years ago,” she says. (Her group presented its findings at ASCRS 2019 with Johnson & Johnson Vision.)7 “We found that the patients who received the mixed-and-matched IOLs had the highest degree of spectacle freedom and the lowest degree of side effects, such as glare and halos. The technologies were complementary.”
Lens Selection Variables
There are several important objective variables that the discerning cataract surgeon must take into consideration when selecting the appropriate lenses for a mix-and-match combination. Some of those include a measurement of the patient’s preferred reading distance, which can be used to adjust the IOL’s near focal point, corneal topography and pupil size.
“Corneal topography and pupil size in different light conditions are important factors,” explains Dr. Vilar. “Some corneas may have subtle irregularities that would at first contraindicate a high-add implant. However, a low-add or EDOF IOL may be suitable in these eyes. Then, placing the high add in the other eye would reduce the chance of photic phenomena. Patients with large pupils in mesopic conditions may experience worse dysphotopsias, especially at night and while driving. Similarly, the low-add or EDOF IOL in the dominant eye may reduce the chance of dissatisfaction.”
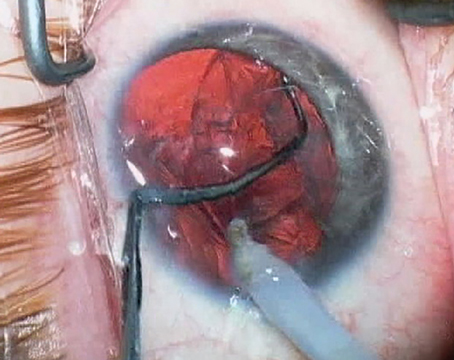
Some surgeons believe that eyes with corneal irregularities, such as those that have undergone previous refractive surgery, may fare better with a zero-aberration IOL, such as the enVista (Bausch + Lomb), which can compensate for some levels of IOL decentration.
Dr. Vilar cautions surgeons to remain aware of eye dominance when selecting lenses. “Eye dominance is a subjective test,” he says. “It often changes after the surgery, which may exacerbate photic phenomena if the high-add lens ends up in the dominant eye. Also, because each eye is set for a different near focus, some activities for near vision, such as reading for extended periods of time, may be more difficult. Typically, it’s advised to place the lens with less add power in the dominant eye since most uncomfortable photic phenomena happen for distance vision, and these lenses are better tolerated.”
Patient Counseling
The other equally important aspect of lens selection is a subjective one. Dr. Vilar says he believes the key to success with presbyopia-correcting lenses is the surgeon’s ability to clearly explain to patients what they should expect from their vision after surgery.
“I usually reserve the mix-and-match approach for patients who demand high visual quality, those who often drive at night and those who insist on a high level of spectacle independence,” he says. “I explain to patients that there’s no guarantee that they’ll have no photic phenomena, but they’re likely to be tolerable. Additionally, I tell patients they may need spectacles for activities with near vision such as reading for long periods. If they accept these drawbacks, I go the blended implantation route.”
Dr. Donaldson agrees that a thorough explanation of visual expectations is important, but she also recognizes that this isn’t an easy task. “We could sit with patients all day long and go through every lens option, but we don’t really have time to do that and the patient isn’t equipped with the full knowledge base to make the decision,” she says. “As surgeons, it’s our job determine the patient’s visual needs and expectations for cataract surgery. We can then use this knowledge to make the best lens choice for our patients. I always explain to patients that cataract surgery is a process involving two eyes, so we do the first eye and evaluate the results and use that information to make any adjustments and modifications for lens choice in the second eye.
“I never tell patients an outcome will be 100 percent, but I do tell them we’re trying to give them the best range of vision possible and freedom from glasses,” she continues. “Some patients may still need light reading glasses for very small print. But if they’re 100-percent free of glasses, they’re extra happy. We try to under-promise and over-deliver.”
In addition to educating the patient on their lens options and what to expect, it’s important to listen to and learn about him or her. Dr. Donaldson says that “learning about our patients’ lifestyles, occupations and pastimes allows us to best assess their visual needs so that we can combine lenses to meet our patients’ expectations for cataract surgery.”
Dr. Donaldson says that those who are looking for the highest degree of spectacle independence, more range of vision or want the possibility of altering second lens choice are good candidates for receiving different, complementary multifocal lenses.
She adds that patients who may not be the best candidates for the mix-and-match approach include those who can’t spend the extra money for multifocals; those who like wearing their glasses or aren’t interested in spectacle freedom; and those who say they won’t tolerate any degree of halo or glare from a multifocal lens. “Some patients might know family members who were extremely happy with their refractive surgery, but sometimes you’ll have a patient come in whose family member or friend had a bad experience, and they’re afraid of that technology,” she says. “These experiences may also affect how satisfied your patient is.”
Making Compromises
“Fortunately, the evolution of IOL development has provided us greater functionality with decreased side effects such as glare and halos,” says Dr. Donaldson. “However, despite these advances and numerous multifocal and EDOF lens options, we still often need to combine lens options to achieve patient satisfaction. The original mix-and-match combination—mini monovision with standard IOLs—is still the number-one way we allow patients to have more spectacle independence after cataract surgery. Patients achieve high levels of satisfaction with this combination.” REVIEW
Dr. Donaldson discloses financial relationships with Alcon, Johnson & Johnson and Bausch + Lomb. Dr. Vilar receives lecture fees from Alcon.
1. Nuijts RM, Jonker S, Kaufer R, et al. Bilateral implantation of a +2.5 D multifocal intraocular lens and contralateral implantation of +2.5 D and +3.0 D multifocal intraocular lenses: Clinical outcomes. J Cataract Refract Surg 2016;42:2:194-202.
2. Gundersen KG, Potvin R. Comparison of visual outcomes and subjective visual quality after bilateral implantation of a diffractive trifocal intraocular lens and blended implantation of apodized diffractive bifocal intraocular lenses. Clin Ophthalmol 2016;10:10:805-11.
3. de Medeiros AL, de Araújo Rolim AG, Motta AFP, et al. Comparison of visual outcomes after bilateral implantation of a diffractive trifocal intraocular lens and blended implantation of an extended depth of focus intraocular lens with a diffractive bifocal intraocular lens. Clin Ophthalmol. 2017;11:1911-1916.
4. Hayashi K, Sato T, Igarashi C, et al. Comparison of visual outcomes between bilateral trifocal intraocular lenses and combined bifocal intraocular lenses with different near addition. Jpn J Ophthalmol 2019;63:6:429-436.
5. Vilar C, Hida WT, de Medeiros AL, et al. Comparison between bilateral implantation of a trifocal intraocular lens and blended implantation of two bifocal intraocular lenses. Clin Ophthalmol 2017;1:11:1393-97.
6. Mendicute J, Kapp A, Lévy P, et al. Evaluation of visual outcomes and patient satisfaction after implantation of a diffractive trifocal intraocular lens. J Cataract Refract Surg 2016;42:2:203-10.
7. Kontos MA, Donaldson KE, Trattler WB, et al. Custom cataract surgery: Matching lens-based presbyopia correction for personalized vision. Presented at ASCRS 2019, May 4, 2019.