My work as a consultant to the pharmaceutical and medical device industries provides me with a unique perspective on emerging technologies. Looking back over the past two decades at the significant advances that have occurred in drug development, lasers and surgical technology made me wonder about what lies ahead. It might surprise you to know that researchers worldwide have been quietly working away at deciphering the genomics and molecular pathways of the human cell; this will radically challenge how we think about and treat the most common ophthalmic diseases. From the front to the back of the eye, and everything in between, the future of our profession is about to change.
My essay here could not, and does not attempt to, be all-inclusive of every technology and advance on ophthalmology’s horizon. Here are some of the ones I find intriguing.
Cataract
It is probably not necessary to review the data on one of the most intriguing emerging technologies in ophthalmology, namely the femtosecond laser, to place it in its proper perspective. The device, which has been used successfully in excimer laser refractive surgery to create the corneal flap, has crossed over to cataract surgery. The high costs associated with its adoption (upwards of $600,000 for the laser including its annual service contract and supplies) limits its availability to all but the largest of practices or surgical centers. Combined with the inability to recoup the costs through reimbursement, limited experience and a paucity of studies proving efficacy (Does it really perform the steps of cataract surgery better or as well as an inexpensive set of disposable instruments?) Despite this, almost a third of cataract procedures may have been performed with this laser to make the corneal incision, open the lens capsule and fragment the crystalline lens. There is a big push by the major players to advance this technology, leaving little doubt that it will change the way we perform cataract surgery in the future. The latest selling points for the technology, according to manufacturers’ claims, include: Bausch + Lomb’s Victus curvilinear corneal docking system; LensAR’s precise three-dimensional measurement of intraocular lens tilt/decentration and lens-cutting protocols to reduce the ultrasound energy required for lens fragmentation; and Alcon’s LenSx laser’s improved visualization that uses its computer’s image- guided system. Abbott Medical Optics recently acquired OptiMedica’s Catalys which features a patient docking Liquid Optics interface guidance system that provides a clear optical path for the OCT and laser. What is missing from all of these devices is the ability to emulsify, extract the lens and replace it with an IOL. When we see that module, rapid adoption will surely follow.
One of the important additions to the refractive cataract procedure is the ability to measure, in real time, the refractive aberrations of the eye at the time of cataract surgery. The
WaveTec VerifEye for the ORA System provides intraoperative wavefront aberrometry that potentially could improve patients’ refractive outcomes. As more and more patients demand clear, uncorrected acuity following surgery, this technology may yet find a role that would encourage its widespread adoption.
New intraocular lenses that correct refractive error, ocular aberrations and presbyopia are on the horizon, and many of the lenses already in the pipeline are finally receiving Food and Drug Administration approval. Recent approvals include the AcrySof Toric IOL, Tecnis Toric 1-Piece IOLand Trulign Toric IOL. The real advances in IOL design would of course offer the patient a truly accommodative lens. The hurdles from a design and regulatory standpoint of developing an IOL “cure” for presbyopia are not inconsequential; nonetheless the search for the holy grail continues.
Elenza is a next-generation, electronic accommodating IOL that is designed to provide a complete visual range, from near, intermediate and distance, what its maker calls an “AutoFocal” lens. This electro-active IOL uses an integrated circuit and a micro-sized power-cell with an expected 50-plus year rechargeable life, to create smart optics; and a proprietary combination of liquid-crystal chemistry, that in milliseconds automatically adjusts focusing power electronically to maintain constant in-focus vision. Sounds pretty neat to me, but what digital device today is just as good in five years? Have they thought about obsolescence? And if the battery still works in five years, what happens if the electronics fail?
Perhaps the establishment of the Medical Device Innovation Consortium (mdic.org), with its unique partnership between the FDA and private enterprise, may make some headway in developing regulatory protocols that will streamline the time it takes to bring a medical device to the public. With few of the major players yet to get onboard, only time will tell whether or not this noble effort succeeds. Stay tuned.
Cornea
If IOLs do not solve the problem of presbyopic correction, perhaps inlays will. ReVision Optics intracorneal Raindrop near vision inlay is a microscopic hydrogel lens for the correction of presbyopia that, after implantation under a femtosecond laser-created flap, creates a prolate-shaped cornea. The AcuFocus Kam-ra Intracorneal inlay uses a pinhole to provide uncorrected near vision. Remember when they sold those as glasses? Likewise the Presbia Flexivue Microlens, implanted under a femtosecond-created flap using Presbia’s proprietary insertion tool.
One of the greatest advances in the treatment of keratoconus and ectatic corneas has been the application of riboflavin, or vitamin B2, combined with excitation by a 370-nm wavelength of ultraviolet-A light. When activated by UV-A light, riboflavin (from the reduced form of the sugar, ribose, combined with its yellow oxidized “flavin”) creates new bonds between adjacent collagen strands within the corneal stroma (cross-linking). Avedro’s KXL System for accelerated corneal crosslinking, uses its investigational LASIK Xtra integrated illumination system to apply the appropriate amount of UV-A following the creation of a corneal flap and application of riboflavin. All we need now is to get the FDA to agree to this treatment modality.
What advances can we expect in the diagnosis of corneal infections? Most clinicians believe that they can adequately tell the difference between a bacterial and a viral keratoconjunctivitis just by looking. They may be sadly mistaken. More than 90 percent of all conjunctivitis is treated with antibiotics, yet more than half may be viral in origin. The AdenoPlus, RPS rapid diagnostic detector is accurate in more than 89 percent of cases and is quick and easy to use. Stop guessing, and just do the test.
Glaucoma
New approaches we are seeing in the treatment of glaucoma, which include both new drugs and surgical devices, are rooted in a new understanding of how glaucoma ultimately damages retinal ganglion cells. Significant strides are being made in the neuroprotection of RGCs. Here is a little background and a look at some of the more interesting approaches.
Apoptosis is programmed cell death. It can be initiated by both an extrinsic pathway, which includes a number of apoptosis-inducing ligands, or by intrinsic pathways that are activated after the loss of pro-survival signals from neighboring retinal, optic nerve or brain neurons. Downstream regulation of extrinsic and intrinsic pathways of apoptosis initiators are becoming interesting and viable targets for glaucoma therapies. Nitric oxide (NO) is an important messenger in intra- and extracellular communication. NO is formed from L-arginine by nitric oxide synthase (NOS). NOS is well-distributed in the trabecular membrane. This molecule is implicated in vasodilatation, trabecular membrane contractility, neurotransmission, neurotoxicity, inflammation and anti-apoptosis of RGCs (neuroprotection).
RGC-targeted glaucoma treatments now in clinical trials include medications injected into the eye that deliver survival and growth factors to RGCs, also useful for stroke and Alzheimer’s disease, such as cytidine-5-diphosphocholine; and the adenosine agonist CHA, which has been shown to significantly increase conventional outflow facility. Mechanical approaches such as electrical stimulation of RGCs delivered via tiny electrodes implanted in contact lenses or other external devices are also under investigation. Memantine, an NMDA glutamate receptor antagonist that blocks glutamate excitotoxicity, is the first drug approved for use as a neuroprotective agent in moderate to severe Alzheimer’s dementia. Evidence of its usefulness in glaucoma is mounting as we elucidate protective effects against RGC loss. Human trials of stem cell therapies are also in the planning stages.
Drugs such as brimonidine, which activate alpha-2 adrenoreceptors, first showed promise as a neuroprotective, but recent data suggests otherwise. Caspase inhibition increases retinal cell survival, and a siRNA-based caspase inhibitor is now in human testing in a multicenter trial for non-arteritic ischemic optic neuropathy.
We all know that the optic nerve, being derived from CNS neurons and covered with CNS myelin, does not regenerate. Glial cells release inhibitory molecules that actively signal RGC axons to stop growing. A number of these molecules have been identified and drugs are being developed to overcome their inhibitory influences. For example, antibodies to the oligodendrocyte-derived protein Nogo are in clinical trials for spinal cord injury, and neurotrophins are a promising class of drugs that have been tested in ALS, Parkinson’s and other neurodegenerative diseases. It is only a matter of time before these advances translate into ways to protect the optic nerve, prevent its degeneration and encourage its regeneration.
Measuring Intraocular Pressure
Intraocular pressure is still one of the pillars of glaucoma management, and better ways of measuring IOP are being developed. Implandata has created a 24-hour intraocular pressure measurement device that offers continuous telemetric measurement of intraocular pressure. The system consists of an implantable micro sensor, which does the pressure sensing, and an external handheld device, which measures and stores the data and transfers energy to the micro sensor telemetrically. The Sensimed Triggerfish Sensor is a soft hydrophilic single-use contact lens, which contains passive and active strain gauges embedded in the silicone to monitor fluctuations in diameter of the corneo-scleral junction. The output signal is sent wirelessly from an antennae that is placed around the eye and connected to a portable recorder through a thin flexible data cable.
The patient wears the device for up to 24 hours; the data is then transferred from the recorder to the practitioner’s computer via Bluetooth technology for immediate analysis. The data collected is said to directly correlate with fluctuations in intraocular pressure. Bye, bye Dr. Goldmann.
Surgeons have revisited the surgical approach to glaucoma. Recognizing that the trabecular meshwork and its juxtacanalicular connections to Schlemm’s canal are the site of much of the resistance to outflow, new micro-invasive glaucoma surgical technologies and improved surgical techniques are being developed to take advantage of this approach. The Glaukos
iStent Trabecular Micro-Bypass is said by its manufacturer to be the first MIGS device to create a permanent opening in the trabecular meshwork (which seems like old news to me); it can be implanted during cataract surgery and is the smallest medical device ever approved by the FDA.
The Ivantis Hydrus Microstent is claimed to be the world’s first “intracanalicular scaffold” for the treatment of primary open angle glaucoma. The Hydrus procedure is said to be less invasive than traditional glaucoma surgery, and can be performed during cataract surgery through the same incision. Roughly the size of an eyelash, the Hydrus Microstent is made from a super-elastic, biocompatible alloy (Nitinol) that has been used in other implantable devices.
Another player exploiting the MIGS approach to glaucoma surgery is Rheon Medical, a start-up affiliated with the Ecole Polytechnique Fédérale de Lausanne. Its EPFL-designed implantable device is considered a “microtap.” Containing a magnetic disk surrounded by a silicon tube, it is designed to rotate around an eccentric axis that compresses the tube, to either a greater or lesser extent. In this way the flow rate through the tube can be adjusted remotely.
AqueSys XEN Gel Stent, which is about the width of a human hair and smaller than the eye of a needle, is made of a permanent, soft, collagen-derived gelatin. Upon implantation, it creates a diffuse outflow of aqueous from the anterior chamber into the non-dissected tissue of the subconjunctival space.
InnFocus-Innovia, the company that created an orbital tissue expander for microphthalmia and anophthalmia, is developing the MIDI-Arrow Glaucoma Device drainage implant. This device consists of a microtube made from SIBS (polystyrene-block-isobutylene-block-tyrene) polyester that is inserted into the anterior chamber of the eye. In one version, the tube shunts fluid into a bleb made in the conjunctiva. In another version, the tube is attached to a plate that receives the shunted fluid while also maintaining the bleb. The third round of clinical trials is already under way.
Retina—AMD
Patients with age-related macular degeneration were told not that long ago that there was nothing that could be done for their disease, and that they could expect to lose vision or go blind. Today, these patients have hope. Advances in the treatment of retinal diseases have occurred at a breathtaking pace. We have witnessed game-changing recombinant antibodies targeting vascular endothelial growth factor, originally used to treat various cancers, being turned on the blinding retinal diseases. The incredible results that we have witnessed in our patients with the use of these molecules are going to be tough acts to follow. However, the landscape is about to change.
Biosimilars and Biosuperiors
The first generation of recombinant antibodies targeting VEGF, that included Macugen (pegaptanib sodium injection), has been largely replaced by the more efficacious Lucentis (ranibizumab). The humanized antibody fragment Lucentis, marketed by Novartis and Roche/Genentech, generated sales of $3.67 billion in the United States in 2011. The full-length therapeutic antibody Avastin recorded sales of $5.6 billion. These are not insignificant drugs. Approved indications for Lucentis include wet AMD, diabetic macular edema and macular edema following central retinal vein occlusion. Patents covering Avastin and Lucentis are going to expire over the next several years. Get ready to witness a nor’easter blowing that will irrevocably change the landscape and pave the way for biosimilar antibodies. The first Avastin biosimilars are already in clinical trials and there are at least 10 others in the pipeline undergoing further development.
What about biosuperiors? The next generation of anti-VEGF antibodies is led by the fusion protein aflibercept, marketed under the name Eylea, which is administered intravitreally every month for three months followed by dosing every eight weeks for two months. Eylea is also indicated for the treatment of patients with macular edema due to CRVO. Another new treatment is Jetrea (ocriplasmin), an intravitreal injection, proteolytic enzyme, which for the first time allows a retinal surgeon a non-surgical alternative to relieve vitreomacular adhesion.
Anti-amyloid therapy, which has already been used clinically in Alz-heimer’s disease, has been shown to protect against retinal pigmented epithelium damage and vision loss in an animal model of AMD.
AMD is characterized by the accumulation of extracellular lipid- and protein-containing deposits between the RPE and Bruch’s membrane. These sub-RPE deposits contain activated components of the complement system (such as C3b and C5b-9), which boost the host defense against invading pathogens. In addition, amyloid P component and proteins such as complement factor H, vitronectin, clusterin/apolipoprotein J, apolipoprotein E (apoE), and amyloid-β (Aβ) have been shown to be involved in the immune and inflammatory responses.
Comparing unique anti-Aβ antibodies, which target the two most common forms of Aβ (i.e., Aβ40 and Aβ42), has shown promise in preserving retinal function and protecting the RPE. Clinical use of anti-Aβ antibodies may have therapeutic value in the treatment of both early and advanced stages of AMD.
Another intriguing set of molecules is the miRNAs (or miRs), which are small, noncoding RNAs that negatively regulate gene expression post-transcriptionally. These molecules play an important role in pathological angiogenesis and oxidative stress, and they trigger the inflammatory and immune responses associated with AMD. Presently there are several miRNAs whose direct involvement in choroidal neovascularization and RPE atrophy has been well-established, and this makes them tempting therapeutics for the treatment of AMD.
Retina—Diabetes
Available interventions for diabetic retinopathy and diabetic macular edema include laser photocoagulation therapy and vitrectomy. Unfortunately, these oft-used therapies primarily target the advanced stages of disease. The biochemical pathways that result in the vascular occlusion and fragility that are the hallmarks of DR have been elucidated. Several biochemical mechanisms—including protein kinase C-β activation, increased VEGF production, oxidative stress, accumulation of intracellular sorbitol and accumulation of advanced glycosylation end products—have been targeted for pharmaceutical intervention. The new goal is to intervene in DR and DME earlier in the disease and provide prophylaxis prior to the development of the neovascular and sight-threatening stages.
Advanced laser systems that facilitate precise treatments for DR include the new OD-OS Navilas Laser System, which incorporates OCT imaging, planning and treatment capabilities in one device. Sounds like a winner to me.
Retinopathy of Prematurity
Many have thought that retinopathy of prematurity was a conquered disease. With more premature babies surviving than ever before, the need for interventions is just as great as in the 1950s. Almost 95 percent of infants born at 23 weeks of gestation, and 40 percent of all infants born prior to 32 weeks suffer from severe multisystem complications. We have recently learned that the driving force in normal fetal development, that is missing in prematurity, is sufficient production of growth factors. Insulin-like growth factor I (IGF-I) has been shown to be associated with several of the most serious complications, namely, ROP, bronchopulmonary dysplasia, intraventricular hemorrhage, necrotizing enterocolitis and impaired brain growth. Premacure, a pharmaceutical company based in Uppsala, Sweden, has been working to commercialize an Insulin-Like Growth Factor 1 (IGF-I) with or without its natural binding protein, IGFBP-3, which has been shown to prevent the complications of preterm birth. (Premacure was recently acquired by Shire, PLC, which is continuing the Phase II study of protein replacement therapy.)
Retina—Devices
Quantel Medical, a manufacturer of diagnostic ultrasonic devices, released its new ultrasonic probes for A and B scans recently and has received FDA approval for its Vitra Multispot laser, which provides advanced pattern-scanning technology for retinal treatments.
Clarity Medical Systems, manufacturer of the RetCam3, a retinal imaging device with its integrated optical systems, is said to enhance the clinician’s ability to diagnose, manage and treat retinal diseases.
Oraya Therapeutics uses highly targeted, low-voltage X-rays to inhibit and prevent the growth of choroidal neovascularization associated with wet AMD. Oraya Therapy Stereotactic Radiotherapy is considered a first-line treatment designed to maintain or improve vision while reducing the required number of intravitreal anti-VEGF injections.
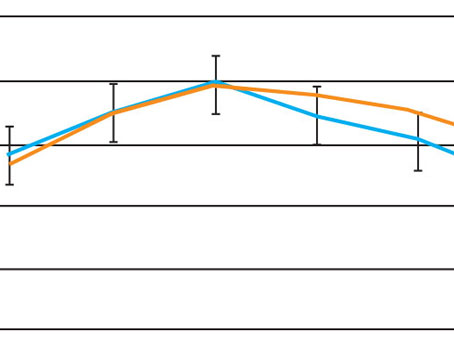
Recently released two-year data from the INTREPID study confirmed a 25 percent mean reduction in anti-VEGF injections over two years in a broadly inclusive cohort of non-naïve wet AMD. Patients identified in the first year of the study as ideal response candidates maintained an impressive 45 percent mean reduction in anti-VEGF injections through the two-year visit, with superior vision to the non-treated group.
Drug-Delivery Systems
One of the major challenges facing ophthalmologists in the treatment of glaucoma is the ability to deliver glaucoma drugs consistently and uniformly into the anterior segment where they are needed. Patient compliance is the most common issue, as well as the need to overcome pharmacologic constraints. The bioavailability of drugs delivered topically is quite poor; only 5 percent or less actually makes it into the eye with topical delivery. Though long the preferred method of drug delivery, primarily because there haven’t been many other options, we are now recognizing that it is mostly ineffective. The eye has several barriers—corneal, blood aqueous and blood vitreous—that additionally make drug penetration inefficient. Sustained drug delivery has been successful for up to six months with intravitreal implants such as Vitrasert, and up to three years with Retisert and Iluvien. There are, however, no available systems for long-term drug delivery to the anterior segment of the eye. Studies presently under way include the use of mucoadhesives, viscous polymer vehicles, transporter-targeted prodrugs, and receptor-targeted functionalized nanoparticles. Older methods are being revisited for use in the eye, including iontophoresis, the lowly punctal plug and contact lens delivery systems. A few of these might be useful in treating diseases affecting the back of the eye as well.
Contact Lens
Lets take a look at the low-tech contact lens. Hydrogels, when saturated with a drug, colloidal nanoparticles or molecular imprinting, can be easily manufactured, placed on the eye, removed and replaced as necessary. The challenges of lens migration, insufficient oxygenation of the cornea, foreign body and risk of infection cannot be overlooked, however.
Amorphex Therapeutics has developed its own Topical Ophthalmic Drug Delivery Device, which is reminiscent of the old Ocusert (pilocarpine ophthalmic). Using its proprietary knowledge of polymer formulations, the company has successfully incorporated a wide variety of drugs into its polymer metrics: prostaglandins; timolol; prednisolone; dexamethasone; brimonidine; and ibuprofen. In vitro drug release studies confirm the ability of these polymers to create consistent drug-release profiles over many months. Simply slip this piece of plastic under the patient’s upper eyelid, and she can forget about her drops. Sounds easy, doesn’t it?
If you can’t get the drug onto the eye, maybe you can stop the drug from getting off of the eye. That concept is the basis for the use of punctal plugs as drug delivery systems. QLT Inc. has developed its proprietary punctal-plug drug delivery technology that potentially could deliver a controlled and sustained release of a variety of drugs to the eye through the tear film. The punctal plug, impregnated with the medication to be delivered and placed into the eyelid punctum, could be retained for the desired treatment duration and removed or replaced as necessary.
If these methods have enough spark to excite your interest, then perhaps the EyeGate II Delivery System, a method of delivering corticosteroids using iontophoretic treatment, might. Iontophoresis is the method by which an inert electrode electrolyzes water to produce hydroxide or hydronium ions. These ions can be used to propel charged molecules, such as steroids, through tissues. The method has demonstrated efficacy in its Phase III study where topical multiple daily dosing with prednisolone was compared to once-weekly treatments with the device. The endpoints were equally met in both groups.
Neurotech boasts an intriguing Encapsulated Cell Technology implant system, which continuously delivers recombinant biotherapeutics for up to two years. This technology uses an immortalized and transformed RPE cell line, which can secrete all modern classes of biotheraputics: cytokines; monoclonal antibodies; antibody Fabs; single chain Fv; and other scaffolds at a rate of 50 pgm/cell/day. The device is made of a semi-permeable polysulphone exterior capsule and internal scaffold of polyethyleneteraphtalate yarn. The cells grow within the hollow capsule, and when implanted in the vitreous, allow for drug diffusion through the pores in the capsule, which can be engineered to release specific amounts.
Novel Therapeutics
Shedding light on the biochemical pathways that signal transcription has been furthered by a new understanding of the regulatory roles of small molecules that turn genes on and off. With each new discovery of a pathway, such as the cytokines that trigger inflammation, comes a new potential drug target. Because these pathways are universal to human cells, targeting drugs which may be useful in diseases such as rheumatoid arthritis and polycythemia vera may also have topical applications for dry eye.
Kinases are enzymes whose primary job is to transfer phosphate groups from ATP (remember that molecule as the “currency” of the cell’s metabolic fuel requirements?) to a five- or six-carbon sugar, protein or lipid. Phosphorylation, well known for some time for its role in glycolysis, also plays an important role in turning pathways on and off. To date, hundreds of molecules targeting a specific kinase are undergoing investigation for their potential to treat disparate diseases, from solid tumors to atopy. A complete discussion of this topic is well beyond the scope of this article, but a few, novel therapeutics deserve mentioning.
Dry-Eye Therapies
Human tear film fluid is composed of a complex mixture of proteins, glycoproteins, lipids and small molecules. Several tear biomolecules have been shown to be excellent biomarkers for autoimmune diseases and infections, and as such could be useful for diagnostics.
It is difficult to analyze tears; after all, we only produce microliters of the precious liquid. The time and expense required to analyze a sample with ELISA testing, or by using a laboratory with expensive automated devices, precludes routine use. Rapid, highly reproducible assays for tear proteins, tear osmolarity and tear molecules could be of benefit in making a quick diagnosis. TearLab Diagnostics has FDA approval to market its osmolarity tester as an accurate biomarker to assess the extent of dry-eye disease. The desktop handheld device is easy to use, fast and accurate, and needs only 50 nanoliters of tears to assess tear film osmolarity. Hyperosmolarity is a known marker for dry eye; a difference between the two eyes is also supportive in making the diagnosis. Measuring other molecules in tears such as lactoferrin, which is a tear-specific protein that is reduced in keratoconjunctivitis sicca, may be beneficial when making a diagnosis.
One of the more intriguing new drugs for dry eye is one that is presently in Phase III testing. SARcode Bioscience (Shire) is evaluating the safety of a topically applied 5% solution of Lifitegrast. Lifitegrast is a first-in-class molecule that inhibits T-cell inflammation by blocking the binding of 2 key cellular surface proteins (LFA-1 and ICAM-1). These receptors mediate the chronic inflammatory cascade triggered by T-lymphocytes (CD3). These cells carry the LFA-1 receptor on their surface, which binds to ICAM-1, which in turn initiates the cytokine cascade. Lifitegrast, by blocking the binding to the receptors, prevents T-cell migration into tissues and arrests the trigger for inflammation.
Thoughts for the Future
Medical innovation is alive and well. Supported by generous investment and funding, the right research team, and perhaps a big cash payoff if the drug or device hits, can be just the medicine needed to stimulate development of the next generation of therapeutics. Who better to direct and lead the pursuit of these miracles than the physicians who will use them to treat patients? To succeed, research and development must include physician-led innovation. Patients don’t drive technology, doctors do. This concept, of which I am a strong proponent, was recently supported in a Viewpoint article published in the March 20, 2013 issue of the Journal of the American Medical Association.
If necessity is the mother of invention, then adversity is the mother of innovation. Every time a physician gets frustrated with the inability to treat a patient, the seed for a solution is planted. Traditional academic research may not be the best vehicle to test new devices and drugs. It is difficult to adequately assess, in randomized control trials, the independent impact of an innovation on patient care. The physician who will use the treatment is in the best position to determine efficacy. Let’s face it, our history is awash in physician-led discoveries: looking at a shard of plastic and deciding it could be made into an intraocular lens implant, or figuring out how an ultrasonic device used to clean teeth might be used to remove a cataract.
Physicians must get involved, provide industry with direction, and feed the incubators with new discovery. When that day arrives, our patients will enter an in-office technology suite, and in less than a blink of the eye, have their crystalline lens removed, refractive correction applied, and a custom laser-lathed IOL inserted to restore perfect vision at any distance, with a physician viewing the whole thing on a computer screen. Just dreaming.
REVIEW
Dr. Kershner is a physician innovator, president and CEO of Eye Laser Consulting and a professor and chairman of the Department of Ophthalmic Medical Technology at Palm Beach State College.