Many technological developments that impact ophthalmology come from doctors or researchers within the field. Occasionally, however, advances in other areas become of interest to ophthalmologists. One such technology is 3-D printing, which allows anyone to design and create a three-dimensional object without many of the practical difficulties associated with older manufacturing methods.
Brett Kotlus, MD, a New York City-based oculoplastic surgeon specializing in cosmetic and reconstructive eye and face procedures, has become interested in this technology, and he’s already using it in creative ways to enhance patient care. “3-D printing is not a new technology; it’s actually been around for 30 years,” he says. “It’s become more accessible in the past eight to 10 years because we now have more affordable printers and more materials that we can use in them.”
How 3-D Printing Works
The 3-D printing process, called additive manufacturing, creates a three-dimensional object by depositing layer after layer of material until the finished object is constructed. The process is guided by a computer. “In contrast, traditional manufacturing uses either injection molding to create an object, or so-called reduction technology, which removes layers of material from a block to create a final shape,” Dr. Kotlus notes. “Those approaches can be very time-consuming and expensive when you’re aiming to make something customized or unique.”
Dr. Kotlus explains that 3-D printers use one of two main methods to add successive layers as the object is being created. “One is extrusion, in which the material is pushed out of the tip of a nozzle, much the way a glue gun works,” he says. “Usually, the material used in that situation is melted plastic. The other method is sintering, in which a powder or liquid is deposited one layer at a time; then a light or laser shines on it to harden the material selectively. Either way, the layers add up to create a solid object.
“The limits of this technology come down to what materials are available and the resolution at which current machines can print,” he continues. “It’s now possible to print an object in almost any material. I’ve printed in ceramic and metal, and you can even print in living tissue. One approach to doing the latter is to print a scaffold through extrusion and then populate that scaffold with living cells or tissue. However, other approaches are also being studied right now. As far as how small you can go, I think the resolution is relatively unlimited. I don’t see why we couldn’t do microscopic 3-D printing, similar to the way circuit boards are created.”
Designing Instruments
Dr. Kotlus notes that there are several ways in which 3-D printing could be useful in ophthalmology. “Those uses include prototyping and creating new surgical tools; helping with surgical planning; creating custom implants; and helping patients visualize the potential benefits of a procedure,” he says.
Dr. Kotlus has already used 3-D printing to develop new tools that he can use in his practice. “My practice is exclusively oculoplastic and cosmetic surgery, so I’ve developed instruments to help with the blepharoplasty evaluation and procedure,” he says. One of the tools he’s designed is something he calls an eyelid wand. [See photo, above right.] “It’s a tool you can use to demonstrate to the patient what it would look like if we didn’t offer blepharoplasty, and we left the skin as it is,” he says. “The shape of the wand matches the shape of the eyelid, and it has a ruler on it so I can do my measurements without having to use a separate instrument.”
Dr. Kotlus explains that he hand-draws the shape and dimensions of the object he’d like to create [see example, above] and then hires a designer, who turns it into a digital rendering. “Then I send it to a 3-D printing bureau service in New York City called Shapeways,” he says. “They print it for me in the material I select. The cost to print an item depends on the material used and the size of the item; my instruments range from $8 to $40 per print. One of the advantages of doing it this way is that the bureau can print in materials I can’t, such as stainless steel. At the moment, printers capable of doing that can cost six or seven figures to acquire.”
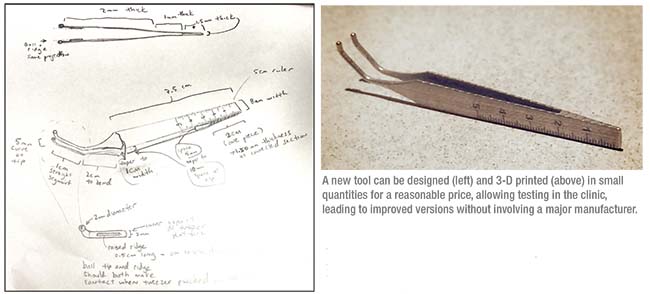 |
Dr. Kotlus says that after he designed his blepharoplasty tool he had 20 copies made using 3-D printing. “I sent them out to some of my colleagues around the country, asking for their feedback,” he says. “They emailed me with suggestions for ways to improve the design, allowing me to modify it based on their feedback. It’s like a crowd-sourced project. Now, instead of having to make a new mold—the way I would if this were an injection-molded tool—I can just have my designer make a change to the file and then print the new version.”
Dr. Kotlus notes that right now, 3-D printing is more cost-effective than the older methods for creating something such as a surgical tool, as long as it’s a custom item or you’re doing a limited run. “If you have to make a large number of items, traditional manufacturing methods will be faster and more affordable,” he notes. “But if you’re looking to create something that’s custom-made, then 3-D printing is often a better way to go, assuming the right material is available.
The reality is, it’s hard to get vendors interested in a custom instrument if they don’t think there will be a sizable market,” he says. “The cost of design and molding—not to mention marketing—can be significant. As a result, it’s often faster and easier to cut out the middleman when creating a niche item, or in the early stages of development, and do it yourself with 3-D printing. Once you have proof of concept it can be easier to approach the bigger industry players.”
Other Uses in Ophthalmology
In terms of helping with surgical planning, Dr. Kotlus describes a couple of ways this technology might be useful. “For example, you can use this technology to print out a duplicate of the patient’s anatomy and look at it in 3-D,” he says. “If you’re doing something that involves cutting or rearranging bones, you can duplicate the patient’s skeletal structure and practice the surgery on the model before you do it on the patient. This helps you to visualize approaches and structures in three dimensions, which may increase your understanding of the problem and can make a procedure go more smoothly.”
In terms of printing custom implants, such as a drug-dispensing device or retinal prosthesis, Dr. Kotlus says the sky’s the limit—in theory. “Whatever we can think of should be feasible, as long as we have the technology to work with the appropriate materials,” he says. “I haven’t personally printed any custom implants because of the limited selection of approved materials to date, although there is one rigid material that’s FDA-approved for craniofacial reconstruction. I own a patent for a custom implant process that uses silicone, but it currently requires the use of injection molding. There are still some hurdles to overcome in terms of creating silicone implants with 3-D printing.”
Dr. Kotlus says 3-D printing can also be used to help patients visualize the probable outcome of a procedure. “I’ve used 3-D imaging for what you might call preoperative morphing,” he explains. “You can show a patient what a chin implant would like, or a change to the nose. With our 3-D imaging software, the images we create can be printed into a physical model that patients can hold in their hands.”
Challenges to Overcome
Dr. Kotlus says a big challenge with this technology is having the capital and resources to develop new materials. “New materials will have to be developed and then approved for medical purposes,” he notes. “For example, let’s say you want to create an intraocular lens. You’d need a material that would be able to withstand the 3-D printing process while maintaining its clarity and shape and size. Obviously, we’re not there yet. The FDA approval process is also in its infancy because medical use of this technology is relatively new. However, they do have new guidelines for medical 3-D printing. The FDA has recognized that this is a growing field that’s going to play a role in medicine.
“Printer resolution may also be an obstacle, depending on what you’re trying to print and the material
 |
| 3-D printing can be used to create custom implants. Above: A custom acrylic chin implant, next to a 3-D printed copy of the patients’ mandible. |
involved,” he continues. “But one of the biggest obstacles is having really useful content to create. It’s easy to say that we can prototype instruments; but if you don’t have a solid idea for an instrument, then the technology will only take you so far. Without that part of the equation, 3-D printing will be of limited use.”
Dr. Kotlus points out one future development that should be particularly useful in the field of medicine: the ability to use multiple materials in the same implant. “For example, if you have a 3-D bioprinter that can use different types of cells, you could potentially print organs,” he says. “That sounds like science fiction, but I think it’s possible. It’s simply a matter of the technology progressing along the same path it has been, and the approvals moving along with it.”
Making the Most of 3-D Tech
Dr. Kotlus notes that 3-D printers have become quite affordable. “You can purchase a 3-D printer that uses plastic for less than $500,” he says. “You can then download models from the Internet that you can print in your home. Or, instead of purchasing a printer, you can go to places that have printers available such as office supply stores or Home Depot and print the files yourself. At Shapeways, the 3-D printing bureau service in New York City that I use, you can browse through models that designers have created; they’ll print it for you and ship it to you.” (Dr. Kotlus notes that he’s created designs of his own that are available through Shapeways, including a model for silver cufflinks, and one for a container in which you can store razor blades. He gets a royalty if one of his designs is used, but he’s also made the files available online so anyone can download them and print them on their own.)
Dr. Kotlus admits that most ophthalmologists probably don’t need this technology in their offices today, given the limited medical uses available so far. “Many dentists now use them in their offices to create dental implants, but in a medical office it’s not really necessary yet,” he says. “If you’re interested in experimenting with the technology, or if you have kids interested in it, that might be a reason to get a device. But professionally, if you’re interested in creating something such as an instrument prototype, it’s probably easier to do it the way I did.
“Already this technology is being utilized more than you might think,” he adds. “The University of Michigan has been creating implants to help children with congenitally narrow tracheas. They’ve implanted them and saved lives, and there have been reports of other successful reconstructive 3-D-printed implants. There’s also a project called ‘E-nable’ that pairs hobbyists who have 3-D printers with children who need prosthetics such as hands. The project provides the blueprints that can create the prosthetic limb; Boy Scout troops and elementary school classes are then able to create those limbs and provide them to children who need them. They can even make them in superhero colors. This program helps these children to integrate and function in a social setting. I think we’ll be seeing more of all of these kinds of uses.
“This is clearly an evolving field,” he concludes. “I’m excited to see what will happen next.” REVIEW



